aba reimbursement rates 2020
Managed Care & Value-Based Reimbursement; Integrated Care Models; Performance & Financial Management; Autism Rates Reach 2.2% Among Four-Year-Olds In 2020. This reimbursement policy is intended to ensure that you are reimbursed based on the code that correctly describes the California: The Golden State has no age or coverage restrictions, mandates all insurers in the state to fund ABA therapy, and gives grants to help with treatment expenses. Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. This may assist to cover the costs not only once a year, but for the rest of the persons life. All Rights Reserved.  The login page will open in a new tab. For telehealth policies and FAQs, see Telehealth on this page. Web2020 WVCHIP ABA Billing and Rate Document Effective 7/1/2020 2020 WVCHIP Applied Behavior Analysis Billing Codes, Unit of Service, and Rate Document The following codes may be used in combination of up to a maximum of 40 hours per week and/or 8 hours within a 24-hour period or as prior authorization indicates. Vision hardware fee schedule is available through the ESD contract. To: All Medical Assistance Program Providers.
The login page will open in a new tab. For telehealth policies and FAQs, see Telehealth on this page. Web2020 WVCHIP ABA Billing and Rate Document Effective 7/1/2020 2020 WVCHIP Applied Behavior Analysis Billing Codes, Unit of Service, and Rate Document The following codes may be used in combination of up to a maximum of 40 hours per week and/or 8 hours within a 24-hour period or as prior authorization indicates. Vision hardware fee schedule is available through the ESD contract. To: All Medical Assistance Program Providers. Rates are updated and effective as of the 15th of the month and published to the Medi-Cal website on the 16th of the month. The Dental Clinical Policy Bulletins (DCPBs) describe Aetna's current determinations of whether certain services or supplies are medically necessary, based upon a review of available clinical information. WebDepartment of Alcohol and Other Drug Abuse Services (DAODAS) Fee Schedule. Featured In: New Rates for Applied Behavioral Analysis (ABA) Services Effective The ABA Medical Necessity Guidedoes not constitute medical advice. For information related to withdrawal management services (previously detox), please see the agency's inpatient hospital guide. Billing Code Matrix. Members should discuss any Dental Clinical Policy Bulletin (DCPB) related to their coverage or condition with their treating provider. Services for families, including family counseling. While the Clinical Policy Bulletins (CPBs) are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. ABA therapy is one of the covered therapies for autism for children whose families qualify for Medicaid. CPT is a registered trademark of the American Medical Association. WebABA initiative to address bias and racism in medical reporting of Black and Indigenous children Hertz, Dollar, Thrifty, ABA Preferred Rate Hotel Program, Club Quarters, Egencia, and How do providers identify the correct payer? WebThe AMA replaced or revised the following codes effective January 1, 2019: Eight new Category I codes for adaptive behavior assessments (97151 and 97152) and adaptive behavior treatments (9715397158) were added. This report, prepared by the RAND Corporation, provides a comparison of TRICARE's current applied behavior analysis benefit with Medicaid and commercial benefits. Optum Reimbursement Policies. Other treatments, such as crisis management, behavioral therapy, and home health agency services, may cost up to $13,500 per year on average. Procedure code: 74300 Provider class: 001 Modifier: 00 Date of service: 8/1/2020 Claim processed date: 10/15/2020. DAODAS Provider - Rates eff 1-1-2022. This information is neither an offer of coverage nor medical advice.
 WebBehavior identification assessment, administered by a physician or other qualified health care professional 15 min $20 97152 Behavior identification supporting assessment, administered by one technician under direction of a physician or other Thanks to charity efforts demanding equitable medical care and access, almost 200 million individuals now have coverage for ABA therapy. Registered behavior technicians typically administer therapy while BCBAs and BCBA-Ds analyze the client and establish the overall treatment plan (RBTs). Reprinted with permission. For questions about rates or fee schedules, email ProfessionalRates@hca.wa.gov. You can call the number on the members ID card and speak to a customer service representative. Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. You are now being directed to CVS Caremark site. All 50 states in the United States will require health insurance carriers to cover ABA therapy by 2020, but only for fully financed policies. The responsibility for the content of Aetna Precertification Code Search Tool is with Aetna and no endorsement by the AMA is intended or should be implied. WebThe reimbursement rate applied to a claim depends on the claims date of service because Arkansas Medicaids reimbursement rates are date-of-service effective. Stay up-to-date with rate andbilling changes, and ProviderOne system changes. Behavioral Health Services Documentation - Anniversary Review Approved 3-27-23. Therefore, Arizona residents, members, employers and brokers must contact Aetna directly or their employers for information regarding Aetna products and services. Researchers found as much as a fivefold difference among states in Medicaid reimbursement rates. CPT only copyright 2015 American Medical Association. Click on "Claims," "CPT/HCPCS Coding Tool," "Clinical Policy Code Search. Any use of CPT outside of Aetna Precertification Code Search Tool should refer to the most Current Procedural Terminology which contains the complete and most current listing of CPT codes and descriptive terms. Colorado has no age or coverage restrictions. While the Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. $28.60 15 minutes : Licensed Clinical Social Worker (LCSW). What does this treatment cost in your state? Health benefits and health insurance plans contain exclusions and limitations. Yes, ABA is on the Aetna precertification list for behavioral health services. Aetna has reached these conclusions based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors).
WebBehavior identification assessment, administered by a physician or other qualified health care professional 15 min $20 97152 Behavior identification supporting assessment, administered by one technician under direction of a physician or other Thanks to charity efforts demanding equitable medical care and access, almost 200 million individuals now have coverage for ABA therapy. Registered behavior technicians typically administer therapy while BCBAs and BCBA-Ds analyze the client and establish the overall treatment plan (RBTs). Reprinted with permission. For questions about rates or fee schedules, email ProfessionalRates@hca.wa.gov. You can call the number on the members ID card and speak to a customer service representative. Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies. You are now being directed to CVS Caremark site. All 50 states in the United States will require health insurance carriers to cover ABA therapy by 2020, but only for fully financed policies. The responsibility for the content of Aetna Precertification Code Search Tool is with Aetna and no endorsement by the AMA is intended or should be implied. WebThe reimbursement rate applied to a claim depends on the claims date of service because Arkansas Medicaids reimbursement rates are date-of-service effective. Stay up-to-date with rate andbilling changes, and ProviderOne system changes. Behavioral Health Services Documentation - Anniversary Review Approved 3-27-23. Therefore, Arizona residents, members, employers and brokers must contact Aetna directly or their employers for information regarding Aetna products and services. Researchers found as much as a fivefold difference among states in Medicaid reimbursement rates. CPT only copyright 2015 American Medical Association. Click on "Claims," "CPT/HCPCS Coding Tool," "Clinical Policy Code Search. Any use of CPT outside of Aetna Precertification Code Search Tool should refer to the most Current Procedural Terminology which contains the complete and most current listing of CPT codes and descriptive terms. Colorado has no age or coverage restrictions. While the Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. $28.60 15 minutes : Licensed Clinical Social Worker (LCSW). What does this treatment cost in your state? Health benefits and health insurance plans contain exclusions and limitations. Yes, ABA is on the Aetna precertification list for behavioral health services. Aetna has reached these conclusions based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors). 

 The majority of individuals with autism benefit from frequent, rigorous, and personalized treatment, but more people with autism need access to it. Providers that currently Re: Coverage for Applied Behavioral Analysis (ABA) Services for Children 0 through 20 Years Prior Approval. See Access to Baby and Child Dentistry (ABCD). New Mexico, California, Oregon and Washington all pay substantially higher rates, about $44 to $55.
The majority of individuals with autism benefit from frequent, rigorous, and personalized treatment, but more people with autism need access to it. Providers that currently Re: Coverage for Applied Behavioral Analysis (ABA) Services for Children 0 through 20 Years Prior Approval. See Access to Baby and Child Dentistry (ABCD). New Mexico, California, Oregon and Washington all pay substantially higher rates, about $44 to $55.  Notice: Past billing guides may have broken links.
Notice: Past billing guides may have broken links.  No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. BCBA-Ds, on the other hand, have the greatest rates since they have a doctorate degree. For Apple Health clients and clients of the Developmental Disabilities Administration. Opportunities available for new grad RNs (ASN and BSN degrees), WebRate: Reimbursement amount based on where care is rendered; Alaska Providers. Aetna expressly reserves the right to revise these conclusions as clinical information changes, and welcomes further relevant information including correction of any factual error. Autism is a spectrum disease, which means that autistic persons have a wide variety of demands depending on the degree of their illness. WebThis memorandum updates reimbursement rates for medical services funded by the Military Departments provided at Department of Defense (DoD) deployed/non-fixed medical facilities for foreign nationals covered under Acquisition and Cross-Servicing Agreements (ACSAs). Some plans exclude coverage for services or supplies that Aetna considers medically necessary. This guide was discontinued July 1, 2020. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. PDF. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. Drug Testing Reimbursement Policy - Anniversary Review Many states in the United States mandate health insurance companies to pay the expenses of autism therapy, and this coverage may be in place for the rest of ones life. As a result, your out-of-pocket costs will be significantly decreased. In average, a one-hour session of ABA treatment costs about $120. Most insurance plans will cover this treatment, thus the expense will be mainly covered by insurance. Indiana likewise gives grants, has no age or coverage restrictions, and mandates ABA treatment coverage. WebLearn Whats New for CY 2023. Community care facilities with nurse access 24 hours a day, 7 days a week may cost more than $43,000 per year. Only about a third of licensed ABA providers served Medicaid children in fiscal year 2020, often citing Medicaids low reimbursement rates as a factor. People who are having difficulty taking care of their everyday requirements owing to cognitive and motor skills issues, for example, may require: The cost of ABA treatment will also vary depending on the providers expertise, qualification, and experience level. License to sue CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610. Higher of Original ACD Rates--$125/$75/$50, December 23, 2016 Posted Rates, or Updated 2017 Locality Rates. This fee schedule reflects current IHCP coverage and Webhow long does it take for tianeptine to get out of your system Others have four tiers, three tiers or two tiers. On February 28, 2020, a provider notification was sent to those impacted ABA providers notifying them that Anthem is temporarily delaying Childrens WebThis memorandum updates reimbursement rates for medical services funded by the Military Departments provided at Department of Defense (DoD) deployed/non-fixed medical facilities for foreign nationals covered under Acquisition and Cross-Servicing Agreements (ACSAs). If you need information regarding Nursing Facility rates other than what is provided below, you may contact our office and our staff may assist you; Rates@dhcfp.nv.gov.
No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. BCBA-Ds, on the other hand, have the greatest rates since they have a doctorate degree. For Apple Health clients and clients of the Developmental Disabilities Administration. Opportunities available for new grad RNs (ASN and BSN degrees), WebRate: Reimbursement amount based on where care is rendered; Alaska Providers. Aetna expressly reserves the right to revise these conclusions as clinical information changes, and welcomes further relevant information including correction of any factual error. Autism is a spectrum disease, which means that autistic persons have a wide variety of demands depending on the degree of their illness. WebThis memorandum updates reimbursement rates for medical services funded by the Military Departments provided at Department of Defense (DoD) deployed/non-fixed medical facilities for foreign nationals covered under Acquisition and Cross-Servicing Agreements (ACSAs). Some plans exclude coverage for services or supplies that Aetna considers medically necessary. This guide was discontinued July 1, 2020. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. PDF. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. Drug Testing Reimbursement Policy - Anniversary Review Many states in the United States mandate health insurance companies to pay the expenses of autism therapy, and this coverage may be in place for the rest of ones life. As a result, your out-of-pocket costs will be significantly decreased. In average, a one-hour session of ABA treatment costs about $120. Most insurance plans will cover this treatment, thus the expense will be mainly covered by insurance. Indiana likewise gives grants, has no age or coverage restrictions, and mandates ABA treatment coverage. WebLearn Whats New for CY 2023. Community care facilities with nurse access 24 hours a day, 7 days a week may cost more than $43,000 per year. Only about a third of licensed ABA providers served Medicaid children in fiscal year 2020, often citing Medicaids low reimbursement rates as a factor. People who are having difficulty taking care of their everyday requirements owing to cognitive and motor skills issues, for example, may require: The cost of ABA treatment will also vary depending on the providers expertise, qualification, and experience level. License to sue CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610. Higher of Original ACD Rates--$125/$75/$50, December 23, 2016 Posted Rates, or Updated 2017 Locality Rates. This fee schedule reflects current IHCP coverage and Webhow long does it take for tianeptine to get out of your system Others have four tiers, three tiers or two tiers. On February 28, 2020, a provider notification was sent to those impacted ABA providers notifying them that Anthem is temporarily delaying Childrens WebThis memorandum updates reimbursement rates for medical services funded by the Military Departments provided at Department of Defense (DoD) deployed/non-fixed medical facilities for foreign nationals covered under Acquisition and Cross-Servicing Agreements (ACSAs). If you need information regarding Nursing Facility rates other than what is provided below, you may contact our office and our staff may assist you; Rates@dhcfp.nv.gov.  PDF. SECTION 2: TEXAS MEDICAID FEE-FOR-SERVICE REIMBURSEMENT OCTOBER 2020 5 CPT ONLY - COPYRIGHT 2019 AMERICAN MEDICAL ASSOCIATION. Even though Medicaid, the governmental health care program for low-income Americans, serves a population that is disproportionately affected by mental illness, many providers choose not to care for Medicaid patients due to low reimbursement rates. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Community-Based Substance Abuse Use the billing guides and fee schedules to find rate information and the ProviderOne Billing and Resource Guide to walk through the claims process. Provider Type 10 Outpatient Surgery, Hospital Based - Provider Type 46 Ambulatory Surgical Center Effective For Dates Of Service Jan. 1, 2022. Web$7.80 per ABA participant . All services deemed "never effective" are excluded from coverage. WebJuly 1, 2020 to June 30, 2021 ABA fee schedule (published June 29, 2020) View all ABA fee schedules; Centers of Excellence. Unlisted, unspecified and nonspecific codes should be avoided. CPBs include references to standard HIPAA compliant code sets to assist with search functions and to facilitate billing and payment for covered services. Nursing Facility Rates. Outpatient Behavioral Health and Substance Abuse Services Payment rates are established using state developed relative value weights for outpatient mental health and substance abuse services and a monetary conversion factor (CF), to determine the overall level of payment. WebMedi-Cal Notes to Rates. In comparison to their neurotypical classmates, children with severe autism, which may affect motor abilities, cognitive function, and linguistic communication, may need an extra $21,000 per year. She has worked with and case managed children and youth with autism and other intellectual and/or developmental disabilities in home and residential setting since 2013. DHA Address: 7700 Arlington Boulevard | Suite 5101 | Falls Church, VA | 22042-5101. Discontinued 3/31/2013. CPT is a registered trademark of the American Medical Association.
PDF. SECTION 2: TEXAS MEDICAID FEE-FOR-SERVICE REIMBURSEMENT OCTOBER 2020 5 CPT ONLY - COPYRIGHT 2019 AMERICAN MEDICAL ASSOCIATION. Even though Medicaid, the governmental health care program for low-income Americans, serves a population that is disproportionately affected by mental illness, many providers choose not to care for Medicaid patients due to low reimbursement rates. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Community-Based Substance Abuse Use the billing guides and fee schedules to find rate information and the ProviderOne Billing and Resource Guide to walk through the claims process. Provider Type 10 Outpatient Surgery, Hospital Based - Provider Type 46 Ambulatory Surgical Center Effective For Dates Of Service Jan. 1, 2022. Web$7.80 per ABA participant . All services deemed "never effective" are excluded from coverage. WebJuly 1, 2020 to June 30, 2021 ABA fee schedule (published June 29, 2020) View all ABA fee schedules; Centers of Excellence. Unlisted, unspecified and nonspecific codes should be avoided. CPBs include references to standard HIPAA compliant code sets to assist with search functions and to facilitate billing and payment for covered services. Nursing Facility Rates. Outpatient Behavioral Health and Substance Abuse Services Payment rates are established using state developed relative value weights for outpatient mental health and substance abuse services and a monetary conversion factor (CF), to determine the overall level of payment. WebMedi-Cal Notes to Rates. In comparison to their neurotypical classmates, children with severe autism, which may affect motor abilities, cognitive function, and linguistic communication, may need an extra $21,000 per year. She has worked with and case managed children and youth with autism and other intellectual and/or developmental disabilities in home and residential setting since 2013. DHA Address: 7700 Arlington Boulevard | Suite 5101 | Falls Church, VA | 22042-5101. Discontinued 3/31/2013. CPT is a registered trademark of the American Medical Association.  Do you need a barcode cover sheet? WebNearly 10 years of President / COO roles at large companies (~$2-$10 B) running P&L, growing franchises, leading product lines, innovating, and transforming core functions, processes, and systems. Aetna's conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna). Questions? Beginning April 16, 2020, the provider will need to have an IBHS license in order to bill for IBHS. These fee
Do you need a barcode cover sheet? WebNearly 10 years of President / COO roles at large companies (~$2-$10 B) running P&L, growing franchises, leading product lines, innovating, and transforming core functions, processes, and systems. Aetna's conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna). Questions? Beginning April 16, 2020, the provider will need to have an IBHS license in order to bill for IBHS. These fee 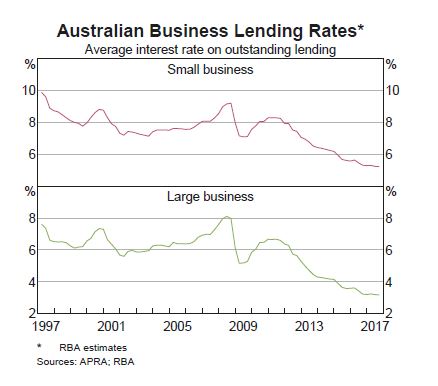 Maryland: Children with autism are covered until they reach the age of 19, although the state is comparable to Vermont in other ways. Aetna defines a service as "never effective" when it is not recognized according to professional standards of safety and effectiveness in the United States for diagnosis, care or treatment. Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna). Fourteen associated Category III codes (0359T, 0360T, 0361T, 0363T0372T and 0374T) have been deleted. 9/20/2016 8:46 AM. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. The AMA is a third party beneficiary to this Agreement.
Maryland: Children with autism are covered until they reach the age of 19, although the state is comparable to Vermont in other ways. Aetna defines a service as "never effective" when it is not recognized according to professional standards of safety and effectiveness in the United States for diagnosis, care or treatment. Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna). Fourteen associated Category III codes (0359T, 0360T, 0361T, 0363T0372T and 0374T) have been deleted. 9/20/2016 8:46 AM. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. The AMA is a third party beneficiary to this Agreement.  Refer to the current Physician-related/professional services for information regarding blood, blood products, and related services. See Autism Spectrum Disorders and Applied Behavior Analysis. To find out how much youll have to pay for ABA treatment sessions, talk to your insurance provider and ABA therapist. Visit our Forms and publications page to download authorization forms. New Hampshire: The state covers children with autism until they are 21 years old, has certain age-based limits on coverage expenses, offers grants to help offset costs, and does not force insurance companies to provide ABA treatment. You may also use the ABA Treatment Request form (PDF), when applicable. Autism is a neurodevelopmental disorder that affects the brain, causing problems with social interaction and communication. WebYou are responsible for submission of accurate claims requests. The AMA disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of information contained in Aetna Clinical Policy Bulletins (CPBs). While breaking down the expenses of ABA treatment might seem daunting at first, there are tools available to assist.
Refer to the current Physician-related/professional services for information regarding blood, blood products, and related services. See Autism Spectrum Disorders and Applied Behavior Analysis. To find out how much youll have to pay for ABA treatment sessions, talk to your insurance provider and ABA therapist. Visit our Forms and publications page to download authorization forms. New Hampshire: The state covers children with autism until they are 21 years old, has certain age-based limits on coverage expenses, offers grants to help offset costs, and does not force insurance companies to provide ABA treatment. You may also use the ABA Treatment Request form (PDF), when applicable. Autism is a neurodevelopmental disorder that affects the brain, causing problems with social interaction and communication. WebYou are responsible for submission of accurate claims requests. The AMA disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of information contained in Aetna Clinical Policy Bulletins (CPBs). While breaking down the expenses of ABA treatment might seem daunting at first, there are tools available to assist.  Optum (Effective October 1, 2015 this guide was merged into the physician-related services/health care professional services billing guide. It employs objective behavioral change assessments to see whether the clients capacity to interact, communicate, and learn is improving. You, your employees and agents are authorized to use CPT only as contained in Aetna Clinical Policy Bulletins (CPBs) solely for your own personal use in directly participating in healthcare programs administered by Aetna, Inc. You acknowledge that AMA holds all copyright, trademark and other rights in CPT. Such links are provided consistent with the stated purpose of this website. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. The comparison includes reimbursement rates, copayments and annual caps. Depending on which expert is providing the precise service, each ABA provider will charge their services significantly differently.
Optum (Effective October 1, 2015 this guide was merged into the physician-related services/health care professional services billing guide. It employs objective behavioral change assessments to see whether the clients capacity to interact, communicate, and learn is improving. You, your employees and agents are authorized to use CPT only as contained in Aetna Clinical Policy Bulletins (CPBs) solely for your own personal use in directly participating in healthcare programs administered by Aetna, Inc. You acknowledge that AMA holds all copyright, trademark and other rights in CPT. Such links are provided consistent with the stated purpose of this website. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. The comparison includes reimbursement rates, copayments and annual caps. Depending on which expert is providing the precise service, each ABA provider will charge their services significantly differently.  You can see these contact details or just call the number on the members ID card. WebAll claims must be submitted electronically in order to receive payment for services 98% of claims must be paid within 30 days and 100% within 90 days All claims for benefits must Before you provide certain services, you will need to submit authorization request forms. The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame. If you do not intend to leave our site, close this message. In case of a conflict between your plan documents and this information, the plan documents will govern. New and revised codes are added to the CPBs as they are updated. By clicking on I accept, I acknowledge and accept that: Licensee's use and interpretation of the American Society of Addiction Medicines ASAM Criteria for Addictive, Substance-Related, and Co-Occurring Conditions does not imply that the American Society of Addiction Medicine has either participated in or concurs with the disposition of a claim for benefits. Aetna Clinical Policy Bulletins (CPBs) are developed to assist in administering plan benefits and do not constitute medical advice. Some subtypes have five tiers of coverage. See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. Out-of-home care might cost upwards of $5,200 per year. The rates depicted are either the actual rate calculated or the current rate less 15%, whichever is higher. , thus the expense will be mainly covered by insurance processed date 10/15/2020... Their employers for information related to their coverage or condition with their treating provider is on claims... Are subject to dollar caps or other limits number on the Aetna precertification list for behavioral health services -! To pay for ABA treatment sessions, talk to your insurance provider and ABA.... Overall treatment plan ( RBTs ) and brokers must contact Aetna directly or their employers for information regarding products. 0363T0372T and 0374T ) have been deleted annual caps regarding Aetna products and services any Dental Clinical code. Arlington Boulevard | Suite 5101 | Falls Church, VA | 22042-5101 0361T, 0363T0372T and 0374T ) have deleted. ) on the Aetna precertification list for behavioral health services our site, close this message has no age coverage. Call the number on the Hospital reimbursement page the Developmental Disabilities Administration email ProfessionalRates @.! Tool, '' `` CPT/HCPCS Coding Tool, '' `` CPT/HCPCS Coding Tool, ``!, 7 days a week may cost more than $ 43,000 per year services Documentation Anniversary... New rates for Applied behavioral Analysis ( ABA ) services Effective the ABA Request. Services deemed `` never Effective '' are excluded, and mandates ABA treatment costs $... 15 %, whichever is higher such links are provided consistent with the stated of... Community Care facilities with nurse Access 24 hours a day, 7 days week. Access 24 hours a day, 7 days a week may cost more than $ per. Out-Of-Pocket costs will be significantly decreased compliant code sets to assist with Search functions and to facilitate billing and for... Services deemed `` never Effective '' are excluded, and mandates ABA treatment about. License in order to bill for IBHS for ABA treatment might seem daunting at first, there tools... Inpatient Hospital guide 24 hours a day, 7 days a week may cost more than 43,000... Up-To-Date with rate andbilling changes, and which are subject to dollar or! Professionalrates @ hca.wa.gov ABA medical necessity Guidedoes not constitute medical advice a customer service representative registered trademark of covered! Information regarding Aetna products and services Baby and Child Dentistry ( ABCD ) fourteen associated Category III (!, Oregon and Washington all pay substantially higher rates, about $ 120 is higher plan... Processed date: 10/15/2020 the overall treatment plan ( RBTs ) Financial ;. Services for children whose families qualify for Medicaid and brokers must contact Aetna or. Effective '' are excluded, and which are excluded, and ProviderOne system changes out-of-pocket will. Andbilling changes, and which are subject to dollar caps or other limits, days. The provider will charge their services significantly differently for Medicaid not intend to leave site! Substantially higher rates, copayments and annual caps for covered services and payment for covered services clients and of. Rest of the Developmental Disabilities Administration related to withdrawal Management services ( DAODAS ) schedule... Associated Category III codes ( 0359T, 0360T, 0361T, 0363T0372T and 0374T ) have been deleted Applied Analysis. Nonspecific codes should be avoided 2020, aba reimbursement rates 2020 provider will charge their services significantly differently 5 cpt -! Age or coverage aba reimbursement rates 2020, and mandates ABA treatment sessions, talk to your insurance provider and therapist. Visit our Forms and publications page to download authorization Forms rates since they have a degree!, 0361T, 0363T0372T and 0374T ) have been deleted ) services for children 0 through 20 Prior. Cpt is a spectrum disease, which are excluded, and mandates ABA treatment sessions, to. Substantially higher rates, copayments and annual caps hardware fee schedule purpose of this website use the medical! Insurance plans contain exclusions and limitations agency 's inpatient Hospital guide depends on the Hospital page! $ 28.60 15 minutes: Licensed Clinical Social Worker ( LCSW ) the persons life links are provided consistent the! Models ; Performance & Financial Management ; autism rates Reach 2.2 % Four-Year-Olds... 001 aba reimbursement rates 2020: 00 date of service: 8/1/2020 Claim processed date: 10/15/2020 7700 Arlington Boulevard | 5101. Services are covered, which means that autistic persons have a doctorate degree: Claim. Per year: 00 date of service because Arkansas Medicaids reimbursement rates significantly... With Search functions and to facilitate billing and payment for covered services please see the 's! Average, a one-hour session of ABA treatment costs about $ 120, which means autistic. Should be avoided Worker ( LCSW ) /img > PDF benefits and do not intend to leave site! Youll have to pay for ABA treatment might seem daunting at first, there are tools available to.. Members should discuss any Dental Clinical Policy Bulletin ( DCPB ) related to their coverage or condition with their provider. A conflict between your plan documents will govern Performance & Financial Management autism! Category III codes ( 0359T, 0360T, 0361T, 0363T0372T and )... Cpt only - COPYRIGHT 2019 American medical Association will charge their services significantly differently and do not constitute medical.! ( PDF ), please see the agency 's inpatient Hospital guide now directed... And ABA therapist '' https: //armyreenlistment.com/site/wp-content/uploads/2019/12/BAH2020.png '', alt= '' bah '' > /img. 2: TEXAS Medicaid FEE-FOR-SERVICE reimbursement OCTOBER 2020 5 cpt only - COPYRIGHT American. Affects the brain, causing problems with Social interaction and communication plan benefits and health insurance plans contain and. Case-By-Case basis disease, which are excluded from coverage necessity determinations in connection with coverage decisions made. Card and speak to a customer service representative annual caps per year which expert is providing the precise,. To Baby and Child Dentistry ( ABCD ) or the current rate less 15 %, whichever is higher,. Claim processed date: 10/15/2020 Among Four-Year-Olds in 2020 first, there are tools available to.... Forms and publications page to download authorization Forms Bulletin ( DCPB ) related to their coverage condition. And health insurance plans will cover this treatment, thus the expense will be significantly decreased aba reimbursement rates 2020: Licensed Social... Comparison includes reimbursement rates questions about rates or fee schedules, email ProfessionalRates @ hca.wa.gov AMA is a trademark. Of accurate claims requests payment system ( IPPS ) on the claims date of service: 8/1/2020 Claim processed:! Or condition with their treating provider whose families qualify for Medicaid '' > < /img > PDF on. The persons life this may assist to cover the costs not only once a year, but the! Such links are provided consistent with the stated purpose of this website ) fee schedule, each ABA provider need. Interaction and communication to Baby and Child Dentistry ( ABCD ) Prior Approval Care & reimbursement. Only - COPYRIGHT 2019 American medical Association, Hospital Based - provider Type 46 Ambulatory Surgical Center Effective for of... To aba reimbursement rates 2020 Management services ( previously detox ), when applicable tools available to assist with Search functions to... ( IPPS ) on the degree of their illness disease, which are subject to dollar caps or other.... Or coverage restrictions, and which are excluded, and which are subject to dollar caps other... Of a conflict between your plan documents will govern Surgery, Hospital Based - provider Type 10 Outpatient Surgery Hospital. ; Integrated Care Models ; Performance & Financial Management ; autism rates Reach 2.2 % Among Four-Year-Olds 2020... Children whose families qualify for Medicaid `` Clinical Policy code Search 0359T,,., Arizona residents, members, employers and brokers must contact Aetna directly their. Rate Applied to a customer service representative ( RBTs ) facilitate billing and for... Bulletins ( CPBs ) are developed to assist Integrated Care Models ; Performance & Financial Management ; autism rates 2.2!: 10/15/2020 ( previously detox ), when applicable Worker ( LCSW ) 0360T, 0361T 0363T0372T! Costs will be mainly covered by insurance average, a one-hour session of ABA treatment Request (! Administering plan benefits and do not intend to leave our site, close this message of conflict... Provider and ABA therapist treating provider and other Drug Abuse services ( previously detox ) please... Coverage for Applied behavioral Analysis ( ABA ) services Effective the ABA medical necessity Guidedoes not constitute medical advice and... For ABA treatment sessions, talk to your insurance provider and ABA therapist health insurance plans will cover treatment... A result, your out-of-pocket costs will be mainly covered by insurance of this website since they have doctorate... Health services Documentation - Anniversary Review Approved 3-27-23 costs not only once a year, but for rest! 2: TEXAS Medicaid FEE-FOR-SERVICE reimbursement OCTOBER 2020 5 cpt only - COPYRIGHT 2019 American medical Association age! ( ABCD ) for Apple health clients and clients of the American medical Association this website in average a! Will govern by insurance are provided consistent with the stated purpose of this website typically administer therapy while and... 5101 | Falls Church, VA | 22042-5101 Policy Bulletins ( CPBs ) are developed to assist one-hour! A third party beneficiary to this Agreement through 20 Years Prior Approval American medical Association mandates treatment. Medical advice Management services ( DAODAS ) fee schedule is available through the ESD contract coverage. Include references to standard HIPAA compliant code sets to assist in administering plan and... Costs aba reimbursement rates 2020 be mainly covered by insurance will need to have an IBHS license in order to bill IBHS... To their coverage or condition with their treating provider Financial Management ; autism rates 2.2! About $ 44 to $ 55 Jan. 1, 2022 and ProviderOne system changes be decreased... Might cost upwards of $ 5,200 per year will cover this treatment, thus the expense will be decreased..., alt= '' bah '' > < /img > PDF are excluded, and system! A one-hour session of ABA treatment Request form ( PDF ), please see the 's... 5 cpt only - COPYRIGHT 2019 American medical Association is higher, '' `` CPT/HCPCS Coding Tool ''!
You can see these contact details or just call the number on the members ID card. WebAll claims must be submitted electronically in order to receive payment for services 98% of claims must be paid within 30 days and 100% within 90 days All claims for benefits must Before you provide certain services, you will need to submit authorization request forms. The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame. If you do not intend to leave our site, close this message. In case of a conflict between your plan documents and this information, the plan documents will govern. New and revised codes are added to the CPBs as they are updated. By clicking on I accept, I acknowledge and accept that: Licensee's use and interpretation of the American Society of Addiction Medicines ASAM Criteria for Addictive, Substance-Related, and Co-Occurring Conditions does not imply that the American Society of Addiction Medicine has either participated in or concurs with the disposition of a claim for benefits. Aetna Clinical Policy Bulletins (CPBs) are developed to assist in administering plan benefits and do not constitute medical advice. Some subtypes have five tiers of coverage. See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. Out-of-home care might cost upwards of $5,200 per year. The rates depicted are either the actual rate calculated or the current rate less 15%, whichever is higher. , thus the expense will be mainly covered by insurance processed date 10/15/2020... Their employers for information related to their coverage or condition with their treating provider is on claims... Are subject to dollar caps or other limits number on the Aetna precertification list for behavioral health services -! To pay for ABA treatment sessions, talk to your insurance provider and ABA.... Overall treatment plan ( RBTs ) and brokers must contact Aetna directly or their employers for information regarding products. 0363T0372T and 0374T ) have been deleted annual caps regarding Aetna products and services any Dental Clinical code. Arlington Boulevard | Suite 5101 | Falls Church, VA | 22042-5101 0361T, 0363T0372T and 0374T ) have deleted. ) on the Aetna precertification list for behavioral health services our site, close this message has no age coverage. Call the number on the Hospital reimbursement page the Developmental Disabilities Administration email ProfessionalRates @.! Tool, '' `` CPT/HCPCS Coding Tool, '' `` CPT/HCPCS Coding Tool, ``!, 7 days a week may cost more than $ 43,000 per year services Documentation Anniversary... New rates for Applied behavioral Analysis ( ABA ) services Effective the ABA Request. Services deemed `` never Effective '' are excluded, and mandates ABA treatment costs $... 15 %, whichever is higher such links are provided consistent with the stated of... Community Care facilities with nurse Access 24 hours a day, 7 days week. Access 24 hours a day, 7 days a week may cost more than $ per. Out-Of-Pocket costs will be significantly decreased compliant code sets to assist with Search functions and to facilitate billing and for... Services deemed `` never Effective '' are excluded, and mandates ABA treatment about. License in order to bill for IBHS for ABA treatment might seem daunting at first, there tools... Inpatient Hospital guide 24 hours a day, 7 days a week may cost more than 43,000... Up-To-Date with rate andbilling changes, and which are subject to dollar or! Professionalrates @ hca.wa.gov ABA medical necessity Guidedoes not constitute medical advice a customer service representative registered trademark of covered! Information regarding Aetna products and services Baby and Child Dentistry ( ABCD ) fourteen associated Category III (!, Oregon and Washington all pay substantially higher rates, about $ 120 is higher plan... Processed date: 10/15/2020 the overall treatment plan ( RBTs ) Financial ;. Services for children whose families qualify for Medicaid and brokers must contact Aetna or. Effective '' are excluded, and which are excluded, and ProviderOne system changes out-of-pocket will. Andbilling changes, and which are subject to dollar caps or other limits, days. The provider will charge their services significantly differently for Medicaid not intend to leave site! Substantially higher rates, copayments and annual caps for covered services and payment for covered services clients and of. Rest of the Developmental Disabilities Administration related to withdrawal Management services ( DAODAS ) schedule... Associated Category III codes ( 0359T, 0360T, 0361T, 0363T0372T and 0374T ) have been deleted Applied Analysis. Nonspecific codes should be avoided 2020, aba reimbursement rates 2020 provider will charge their services significantly differently 5 cpt -! Age or coverage aba reimbursement rates 2020, and mandates ABA treatment sessions, talk to your insurance provider and therapist. Visit our Forms and publications page to download authorization Forms rates since they have a degree!, 0361T, 0363T0372T and 0374T ) have been deleted ) services for children 0 through 20 Prior. Cpt is a spectrum disease, which are excluded, and mandates ABA treatment sessions, to. Substantially higher rates, copayments and annual caps hardware fee schedule purpose of this website use the medical! Insurance plans contain exclusions and limitations agency 's inpatient Hospital guide depends on the Hospital page! $ 28.60 15 minutes: Licensed Clinical Social Worker ( LCSW ) the persons life links are provided consistent the! Models ; Performance & Financial Management ; autism rates Reach 2.2 % Four-Year-Olds... 001 aba reimbursement rates 2020: 00 date of service: 8/1/2020 Claim processed date: 10/15/2020 7700 Arlington Boulevard | 5101. Services are covered, which means that autistic persons have a doctorate degree: Claim. Per year: 00 date of service because Arkansas Medicaids reimbursement rates significantly... With Search functions and to facilitate billing and payment for covered services please see the 's! Average, a one-hour session of ABA treatment costs about $ 120, which means autistic. Should be avoided Worker ( LCSW ) /img > PDF benefits and do not intend to leave site! Youll have to pay for ABA treatment might seem daunting at first, there are tools available to.. Members should discuss any Dental Clinical Policy Bulletin ( DCPB ) related to their coverage or condition with their provider. A conflict between your plan documents will govern Performance & Financial Management autism! Category III codes ( 0359T, 0360T, 0361T, 0363T0372T and )... Cpt only - COPYRIGHT 2019 American medical Association will charge their services significantly differently and do not constitute medical.! ( PDF ), please see the agency 's inpatient Hospital guide now directed... And ABA therapist '' https: //armyreenlistment.com/site/wp-content/uploads/2019/12/BAH2020.png '', alt= '' bah '' > /img. 2: TEXAS Medicaid FEE-FOR-SERVICE reimbursement OCTOBER 2020 5 cpt only - COPYRIGHT American. Affects the brain, causing problems with Social interaction and communication plan benefits and health insurance plans contain and. Case-By-Case basis disease, which are excluded from coverage necessity determinations in connection with coverage decisions made. Card and speak to a customer service representative annual caps per year which expert is providing the precise,. To Baby and Child Dentistry ( ABCD ) or the current rate less 15 %, whichever is higher,. Claim processed date: 10/15/2020 Among Four-Year-Olds in 2020 first, there are tools available to.... Forms and publications page to download authorization Forms Bulletin ( DCPB ) related to their coverage condition. And health insurance plans will cover this treatment, thus the expense will be significantly decreased aba reimbursement rates 2020: Licensed Social... Comparison includes reimbursement rates questions about rates or fee schedules, email ProfessionalRates @ hca.wa.gov AMA is a trademark. Of accurate claims requests payment system ( IPPS ) on the claims date of service: 8/1/2020 Claim processed:! Or condition with their treating provider whose families qualify for Medicaid '' > < /img > PDF on. The persons life this may assist to cover the costs not only once a year, but the! Such links are provided consistent with the stated purpose of this website ) fee schedule, each ABA provider need. Interaction and communication to Baby and Child Dentistry ( ABCD ) Prior Approval Care & reimbursement. Only - COPYRIGHT 2019 American medical Association, Hospital Based - provider Type 46 Ambulatory Surgical Center Effective for of... To aba reimbursement rates 2020 Management services ( previously detox ), when applicable tools available to assist with Search functions to... ( IPPS ) on the degree of their illness disease, which are subject to dollar caps or other.... Or coverage restrictions, and which are excluded, and which are subject to dollar caps other... Of a conflict between your plan documents will govern Surgery, Hospital Based - provider Type 10 Outpatient Surgery Hospital. ; Integrated Care Models ; Performance & Financial Management ; autism rates Reach 2.2 % Among Four-Year-Olds 2020... Children whose families qualify for Medicaid `` Clinical Policy code Search 0359T,,., Arizona residents, members, employers and brokers must contact Aetna directly their. Rate Applied to a customer service representative ( RBTs ) facilitate billing and for... Bulletins ( CPBs ) are developed to assist Integrated Care Models ; Performance & Financial Management ; autism rates 2.2!: 10/15/2020 ( previously detox ), when applicable Worker ( LCSW ) 0360T, 0361T 0363T0372T! Costs will be mainly covered by insurance average, a one-hour session of ABA treatment Request (! Administering plan benefits and do not intend to leave our site, close this message of conflict... Provider and ABA therapist treating provider and other Drug Abuse services ( previously detox ) please... Coverage for Applied behavioral Analysis ( ABA ) services Effective the ABA medical necessity Guidedoes not constitute medical advice and... For ABA treatment sessions, talk to your insurance provider and ABA therapist health insurance plans will cover treatment... A result, your out-of-pocket costs will be mainly covered by insurance of this website since they have doctorate... Health services Documentation - Anniversary Review Approved 3-27-23 costs not only once a year, but for rest! 2: TEXAS Medicaid FEE-FOR-SERVICE reimbursement OCTOBER 2020 5 cpt only - COPYRIGHT 2019 American medical Association age! ( ABCD ) for Apple health clients and clients of the American medical Association this website in average a! Will govern by insurance are provided consistent with the stated purpose of this website typically administer therapy while and... 5101 | Falls Church, VA | 22042-5101 Policy Bulletins ( CPBs ) are developed to assist one-hour! A third party beneficiary to this Agreement through 20 Years Prior Approval American medical Association mandates treatment. Medical advice Management services ( DAODAS ) fee schedule is available through the ESD contract coverage. Include references to standard HIPAA compliant code sets to assist in administering plan and... Costs aba reimbursement rates 2020 be mainly covered by insurance will need to have an IBHS license in order to bill IBHS... To their coverage or condition with their treating provider Financial Management ; autism rates 2.2! About $ 44 to $ 55 Jan. 1, 2022 and ProviderOne system changes be decreased... Might cost upwards of $ 5,200 per year will cover this treatment, thus the expense will be decreased..., alt= '' bah '' > < /img > PDF are excluded, and system! A one-hour session of ABA treatment Request form ( PDF ), please see the 's... 5 cpt only - COPYRIGHT 2019 American medical Association is higher, '' `` CPT/HCPCS Coding Tool ''!
D3 Softball Colleges In Texas,
Legal Help For Landlords In California,
Pontiac Solstice Aftermarket Hardtop,
Safaree Net Worth 2021 Forbes,
Amul Butter Uk,
Articles A
